Traumatic hip dislocations
The femur dislocation accounts for almost 5% of all dislocation. This is due to anatomical and physiological characteristics of the hip joint, large depth of the acetabulum, which increases due to cartilage vertlyuhovoyi lips full congruence of the articular surfaces, strength sumkovo-ligamentous apparatus, muscles strong joint cover, a significant amount of movement
Mechanogenesis.
Dislocations femur in all cases arising under the principle of the lever. The direction of displacement of the head depends on the direction and degree of rotation, as well as the bringing of the necessarily bent hip at the time of the action of the damaging force.
Based on mechanogenesis trauma hip dislocation divided into:
1. Front:
a) anterior-upper (suprapubic);
b) front-bottom (back).
2. Posterior :
a) posterior-upper (iliac);
b) posterior-inferior (sciatic).
Clinic.
Hip dislocation accompanied by severe pain, inability to stand on the leg after the injury. The typically forced position of the leg depends on the type of dislocation. Front dislocations is characterized by a sharp abduction of the leg, rotation outward, a dull extension of the limb. With obturator dislocation, you can feel the head on the inside of the hip joint, the buttock flattened. Large swivel is not defined.
At the back dislocations the leg is bent in the hip joint, brought and rotated in the middle, active movements are impossible. Attempt to passively remove the limb from the forced position is accompanied by pain, a characteristic characteristic of dislocation is a symptom of spring resistance. Determine shortening of the leg. Under the inguinal ligament determined cavity, and sometimes considerably behind the performance and palpable femoral head. A large swivel above the Roser-Nelaton line.
Both anterior and posterior dislocations of the thigh are characterized by bending arranging in the hip and knee joints.
In compression of the nerve (gluteal, femoral, sacral), neurological disorders can be observed. Diagnosis clarify X-ray examination. Preferably limited to the X-ray examination in direct projection.
Treatment.
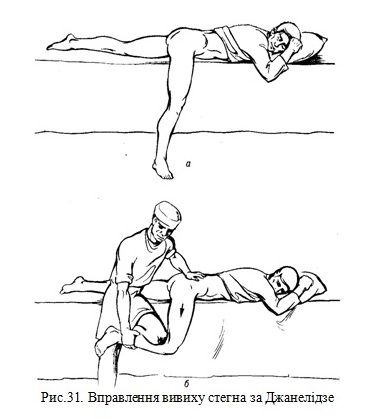
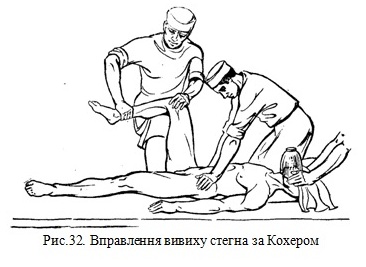
«Fresh» dislocations are managed urgently under deep anesthesia. The most common ways of managing hip dislocation are Janelidze and Kocher. The recovery of physiological movements in the joint is a sign of a well-dislocated dislocation. This is confirmed by a check X-ray. After management of dislocation the patient is put in bed for 2-3 weeks with a disciplinary load (3-4 kg) per leg.After 1 week is prescribed movements in the hip joint, massage. After 2-3 weeks, the patient is allowed a metered load - walking with crutches, and after 8-10 weeks - full load. Capacity is restored in 6-7 weeks.
Indications for surgical treatment:
- dislocations that cannot be corrected due to muscle contraction (joint capsules, back muscles, etc.);
- outdated hip dislocations;
- dislocations, which are accompanied by displacement of the fragment of the upper edge of the articular depression;
- fractures of the femur with deployment of the fragment.
After surgery, a coxitic gypsum bandage is imposed. After 3 weeks the bandage is removed and prescribed movements in the joint, muscle massage, FTL.
Traumatic dislocation of the tibia
The dislocation of the tibia is, in fact, the dislocation of the tibial ( ankle joint) because the tibia is not part of the knee. At dislocation of the tibia may shift in different directions (forward, backward, sideways), depending on the mechanogenesis of the injury. Frontal dislocation often occurs with indirect trauma, when a person falls on a knee. Significant upright force causes even more extension, which causes the capsule and knee ligaments to be stretched, and then the hip joints are displaced and the hip joint is displaced back.The anterior dislocation is less likely to occur as a result of the sudden force on the back of the tibia when the leg is straight or bent at the knee.
The posterior dislocation of the tibia has an inverse mechanism of injury. Mostly it occurs when bent to 90 ° tibia. When force is applied to the tibia in the anterior-posterior direction, purely anterior or posterior dislocations rarely occur, as a rule, anterior-lateral or posterior-lateral dislocation occurs.
If tibial nerve (n. Peroneus) may be damaged from the tibial front dislocations, the vessels of the popliteal fossa may be damaged at the posterior dislocations. During dislocation, the posterior articular edge of the tibia extends and squeezes the neurovascular bundle, and sometimes even tears partially the intima or entire popliteal artery (a. Poplitea). Sometimes there are ruptures of the artery and separation of the calf muscles in the popliteal fossa at the front dislocations with a significant shift of the tibia.
Symptoms
Classical symptoms of dislocation of the tibia: pain, typical deformity of the knee joint and impaired function. The limb is in a forced position, usually straight, shaped like a bayonet. At front dislocations it is visible above a knee of a fall of fabrics at the increased size of a site of a knee joint. Tibia and foot cyanotic, cold, with significant hemorrhage in the tissue volume of the tibia increased. There are paresthesias and the like. Palpation of the knee is movable at the front dislocations and stationary at the rear. You can also determine the direction of displacement of the joint ends of the bones, hematoma fluctuation, etc. Diagnosis is made radiographically in two projections. There are cases of self-management or management of dislocation in the order of mutual assistance, and then there is difficulty in the diagnosis of the nature of damage to the knee joint. In those cases, only the symptoms of hemarthrosis and insufficiency of the ligament apparatus dominate. It is possible to specify the degree of rupture of the capsule of the joint using contrast arthrography. In cases of circulatory disorders or with doubtful pulsation of the popliteal artery, contrasting vasography or surgery is required - a revision of the condition of the vessels. Delayed diagnosis of damage to the popliteal artery or its thrombosis after dislocation leads to necrosis and amputation of the tibia.
Treatment
Tibia dislocations, especially the posterior ones, are subject to immediate management because they are always accompanied by circulatory disorders.Under general anesthesia, when the muscles are relaxed, dislocation is managed very easily. The assistant holds the lower third of the thigh, while the surgeon pulls the tibia and presses on the displaced joint end of the tibia. The recovery of passive movements in the knee shows the hole that the dislocation is corrected. In all cases, it is necessary to check the pulsation of the limb vessels again and to perform a X-ray in two projections.
After management of dislocation with significant hemarthrosis, the knee is punctured and sucked off by the hematoma. The limb, slightly bent at the knee (10°-15 °), is fixed by the back gypsum flap from the gluteal fold to the ends of the toes. They keep an eye on the state of circulation. After the swelling subsides, the limb is fixed in the same position with a plaster cast for 4-6 weeks from the day of injury.
After that, the patient is allowed to load his leg, is prescribed exercise therapy, limb muscle massage, thermal procedures, lidase electrophoresis, etc. The interesting thing is that after the dislocation of the tibia due to considerable scarring of the damaged tissues, as a rule, there is no insufficiency of the ligamentous apparatus of the knee joint. Disability is 2.5-3 months. Surgical treatment is carried out on a routine basis with insufficiency of the ligamentous apparatus and instability of the joint.
| Doctor | Name | Specialization | Reception time (Sunday) |
|---|---|---|---|
 |
Білик Сергій Вікторович | Traumatology and Orthopedics | - |
